#13: Hunger, Appetite, and Weight Loss
Subscribe below to become a health insider!
In This Issue:
Quick Takes: Dr. Zachary Knight on how the brain controls hunger and what it means for weight loss via Huberman Lab
Community Buzz: Interval Walking Training, a wearable for nervous system balance, and more.
Member Spotlight: Leaders at HummingbirdHill made health a shared priority as they participated in Benchmark as a team, to keep each other accountable and support each other's success.
QUICK TAKES
Takeaways from recent content we've discovered
How Your Brain Controls Hunger—and What It Means for Weight Loss
We tuned in to Dr. Zachary Knight on the Huberman Lab podcast, where he explored “The Science of Hunger & Medications to Combat Obesity.” His insights shed light on why we eat the way we do, why keeping weight off is so challenging, and how new medications are changing the game. Below we highlight some of the topics we found particularly interesting.
Why Weight Loss is Hard to Maintain
Fat cells release a hormone called leptin, which signals the brain to reduce hunger. The more body fat you have, the more leptin you produce. In obesity, however, the body can become resistant to leptin, blunting its appetite-suppressing effects.
When you lose fat, leptin levels drop, which triggers hunger. Research shows that for every kilogram of weight lost, appetite increases by about 100 calories per day. At the same time, after weight loss, your body burns fewer calories—around 30 fewer per day for every kilogram lost. The combination of increased hunger and reduced calorie burn explains why sustaining weight loss is particularly challenging.
Genetics, Environment, and the Obesity Epidemic
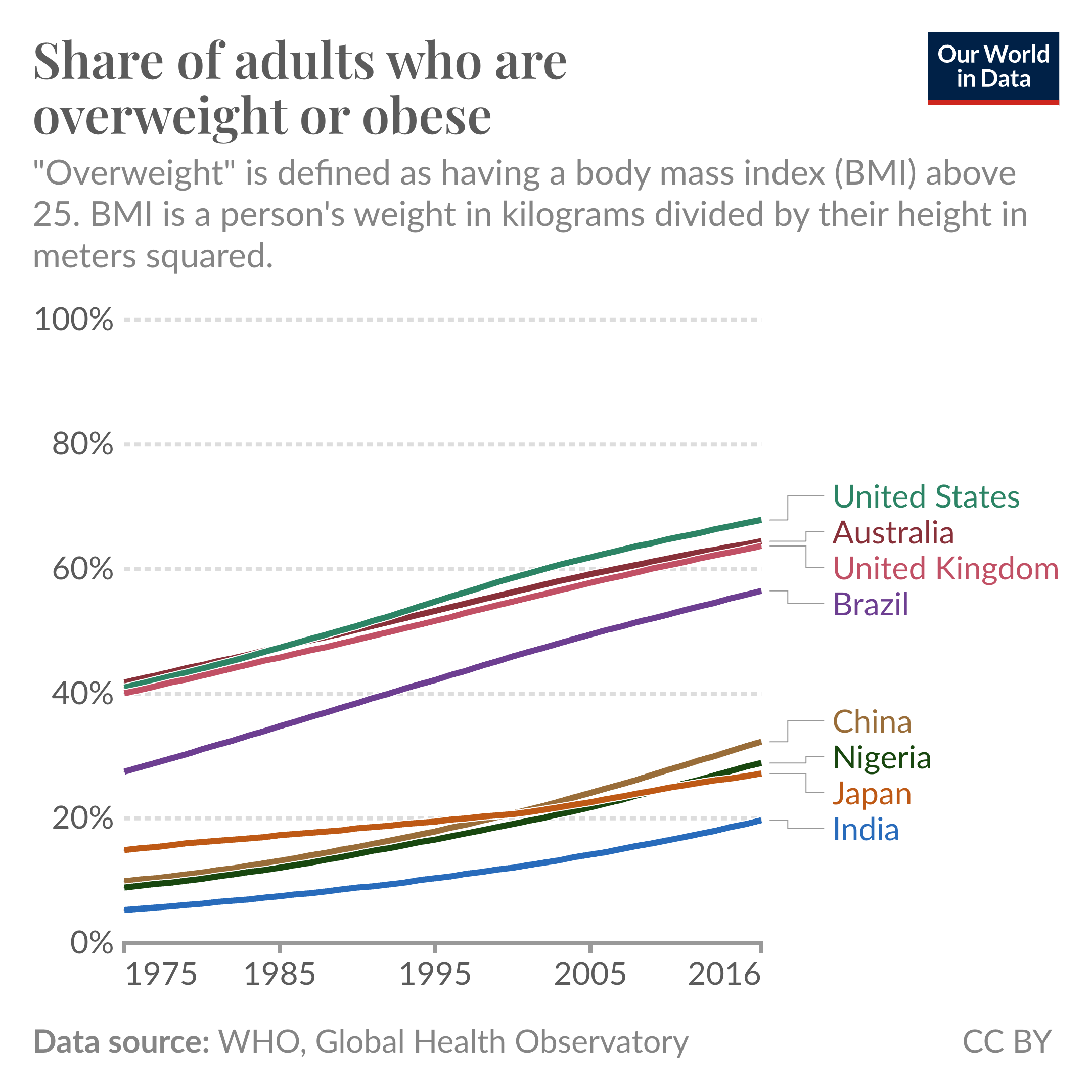
Obesity is strongly influenced by genetics. According to Knight, around 80 percent of the variation in body weight between people is thought to be genetic, the result of more than 1,000 genes linked to hunger and satiety pathways. However, obesity rates have risen dramatically in a short period of time. In the four decades from 1975 to 2016 obesity in the U.S. went from around 40% of the adult population to nearly 70%.
The rapid increase in obesity rates in select countries from 1975 to 2016.
The gene pool doesn’t change this much so quickly, suggesting the environment plays a key role. Dr. Knight explains that some people have a higher propensity to store energy, while others naturally tend to be leaner, and these predispositions interact with a variety of environmental factors. As he puts it, “genetics load the gun and the environment pulls the trigger.”
A variety of environmental factors are likely contributors, but it is very hard to isolate their impact at the population level. The availability of food and variety of options has increased significantly over the past few decades. We have also increased our consumption of ultra-processed foods high in fat, sugar, and refined carbs. These foods activate the brain’s reward system and often override natural fullness signals.
In one study, participants ate as much as they wanted for two weeks on an ultra-processed diet, followed by two weeks on a whole-food diet. They reported both diets as equally tasty, yet consumed far more calories and gained weight on the ultra-processed diet, while losing weight on the whole-food diet. One possible reason? Volume matters. Whole foods take up more space in the stomach for the same calories, helping trigger fullness sooner. Food also trains our brain through its post-digestive effects; for example, we may develop a taste for coffee once we associate it with its energizing lift; similarly, our brains learn that salty potato chips provide instant gratification.
Ultra-processed foods may also blunt “sensory-specific satiety” (our loss of appetite for a specific food group once we’ve had enough) possibly because the brain can’t link these foods to specific nutrients we seek, as it does with whole foods. The result: we keep eating.
Medical innovations for weight loss
GLP-1 receptor agonist drugs mimic the natural hormone “glucagon-like peptide-1”, which helps regulate insulin and appetite by acting on the brainstem. Specifically, GLP-1 reduces appetite by influencing brain regions that control hunger signals, helping people feel full sooner and eat less. Originally developed for diabetes, these drugs, such as semaglutide (Ozempic, Wegovy), can lead to significant weight loss over time and have shown potential benefits for cardiovascular health. Interestingly, studies show cardiovascular benefits from these drugs even before significant weight loss occurs, likely due to anti-inflammatory effects involving the vagus nerve pathway.
Newer medications like tirzepatide (Mounjaro) combine GLP-1 with other hormonal actions to potentially improve effectiveness and reduce side effects like nausea. Research on drugs targeting GLP-1, GIP, and glucagon receptors is ongoing, with some showing promising results in weight reduction and increased resting calorie burn. While nausea can be a common initial side effect, many patients adapt over time. Combining these treatments with resistance training and adequate protein intake can help preserve muscle mass during weight loss, supporting better long-term health
Understanding how the brain regulates hunger, how genetics and environment interact, and how new medications can shift the balance can better equip us for lasting, healthy weight loss.
COMMUNITY BUZZ
Highlights from Benchmark’s community
Pep in Your Step with IWT 🚶
We talk a lot about the value of HIIT (high intensity interval training) for its health benefits and time efficiency. Another thing we love about interval training is its versatility; just about any continuous exercise can incorporate higher intensity intervals, with alternating periods of rest. The latest buzz is around interval walking training (IWT), developed in Japan as an intervention for older adults.
IWT involves 5 or more repeated cycles of 3 minutes of fast walking, followed by 3 minutes of slow walking. The fast interval is at a pace equivalent to about 70% of peak aerobic capacity and “slow” at 40% of peak (or 70% and 40% of max heart rate as a proxy). Several studies discussed here suggest that IWT can positively impact key health metrics, including blood pressure and aerobic capacity, even when compared with continuous walking at lower intensity. Incorporating these moderate intensity intervals can be a great way to boost the benefits of your walking routine.
Calming Touch 😌
Last month we talked about headphones for sound sleep and a headband for meditation. This month, Sam shared a wearable device designed to increase heart rate variability, a key indicator of nervous system balance and stress resilience, and improve relaxation, focus, and sleep. Apollo is a device worn on the wrist or ankle or clipped onto clothing, that provides gentle vibration as a form of touch therapy. Apollo's founder, a psychiatrist and neuroscientist, explains that it was designed with the value of social connection in mind, using our touch response to confer a sense of safety and reset the nervous system. Sam says it helps him fall asleep by providing just enough sensory input to keep his mind from wandering. A device to bring a touch of calm? Feels worth a try.
TV Time 📺
Did you catch us on TV?! Benchmark was featured in a display of corporate event production at its finest, as imagined by talented event planner Carina D'Angelo of Corporate Events Hamilton. Greg Fast, owner of Special Event Rentals offering everything you need to host an event, discussed the exhibit on CHCH Morning Live. Thanks to Cedar Prints (vinyl), AYKAY Group (graphics), Gather Floral & Events (floral), and Kayla Potter (photos).
MEMBER SPOTLIGHT
Featured members and their health journeys
Ian MacFayden of HummingbirdHill
Kyle Kelland of HummingbirdHill
Dave Ovcjak of HummingbirdHill
Ian, Kyle, and Dave earned the spotlight this month! These friends and leaders at HummingbirdHill Homes + Construction asked if they could participate in Benchmark together so they could hold each other accountable, while enjoying a fun experience...and with that, the Benchmark TEAM Physical was born!
Kyle says: "It connected us as a team really well, and made us more dialed in – to our own health and wellness, and as a leadership team. If we’re physically and mentally healthy, we’re driving the business better" Read more...